Search the Community
Showing results for 'pureed foods'.
Found 17,501 results
-
Feeling proud everytime I don't finish the food on my plate

-
People, I try not to give advice, but please don't 'food funeral' yourselves to death: http://www.academia.edu/934287/cognitive_changes_to_preloading_in_restrianed_and_unrestrained_eaters_as_measured_by_the_Stroop_task
-
Its been a week after my 2nd fill and I definitely get fuller with less food now, I can feel a little bit of more restriction but very little. I'm hoping 3rd time's the charm but we will see. I'm well aware it's different for all of us. On a side note my elliptical has made its way back into my bedroom. Hopefully I can make my way onto it

-

@Veronica Page I know I know i'm getting to it ....eventually lol JK thanks

-

-

- Show next comments 237 more
-
-
I know why now I've never chewed my food slowly or thoroughly. It's disgusting.
-
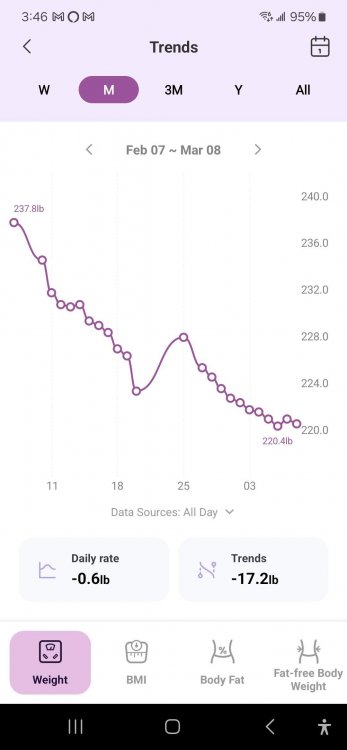
A snapshot of the past 30 days' weight loss. February 7 was the first day of my pre-op diet and surgery was Feb 21. I didn't weigh myself from the 21st thru 24th but you can see the bounce on the 25th due to continued retention of fluids from the hospital. I lost 5.6 lbs last week, but so far only 1.2 lbs this week.
While the weight has been coming off slowly, I did have feedback from my massage therapist on Monday that my inflammation seems much improved. She immediately noticed the difference in my calves, which were always very tight and hard, to the point she would often comment on it as being unusual. This time she was able to get right into the muscle without a struggle, and it was a similar story in my arms, neck and back. Whether it's from the surgery itself or from the complete lack of grains, sugar, and processed foods in my diet for a month, something is working.
-
Those non-scale victories really mean a lot 💪
-
NickelChip reacted to this
-
-
So yeah, now I'm playing the waiting game and patiently awaiting surgery day. In the meantime, I am wondering what food aversions I will end up with. I know after having the gallbladder removal, there are already tons of foods I can't stand or just can't eat all together. So, for my recovery liquids, I decided to not go all out and buy a bunch of things and sit and wait. I suppose broth would be good to keep around and no sugary Jello mix. But beyond that I don't want to spend money on things I may not need or like after. Thinking might be best to wait to see what I can stand while in hospital. Then order or send my husband to get things? If anyone's reading, this...what do you recommend? Did you buy a bunch of things, or wait? 😀
-
2 weeks & 5 days post op and I'm doing great
Gatorade w/protein makes me gag now. I think from having so much of it.
I had the ricotta bake for a few days. I'm in the puree stage but rotisserie chicken, chicken meatballs, cold cuts, & plain tuna don't bother me.
I had a plain old fashioned peppermint and it made me nauseous...
-
I may need to change my name and profile pictures. I assumed I would be struggling to drink water and protein shakes and eating tiny food portions but that's not the case. So far, no nausea. No feeling of food restriction. I guess I should be happy that I can eat comfortably with no appetite and so I'm banking on the surgery itself to do it's part changing my setpoint, metabolism, insulin resistance etc. In 10 days I will move into regular food phase. Maybe then the restriction may kick in.
-
Less than a week before gastric bypass surgery. I'm nervous but excited. Been lurking here for a while, reading. I'm about ready as I'm going to get. Down 20 pounds in 3 months. A ton of pre op testing done and cleared. Food/drinks, chewable vitamins, protein, meds bought. On 2-week preop diet now which includes 2 protein shakes a day along with 3 ounces lean protein and 2 1/2 C. non starchy veggies and is totally do able for me. Clear liquid day before surgery. A full sugar Gatorade night before and again 2 hrs before arriving at the hospital. Interesting how different everyone's diets are depending on your doctor.
I'm optimistic all will go well. Good luck to the April surgeries happening this month and to all that are going through the process. {{hugs}}
-
Finally have my surgery scheduled as of a couple days ago. For 3 weeks prior to phone appointment I was on a diet of 2 meal replacement shakes and 1 lunch under 500 calories only consisting up a small portion of lean meats and green veggies. Successfully loss 23lbs. Now that my surgery is scheduled the surgeon put me on 3 meal replacements a day and 0 food consumption. Also, I officially quit smoking about 5 days prior to that appt. First day on this diet and I don't honestly know how I feel. I'm hungry but I'm also stressed about so many things with and without the surgery I don't even want to eat. I'd rather smoke if you want me to be honest. That is effecting me more than anything probably because I am stressed. This surgery is my whole life savings. Feel like I'll get all the way there and something will cause the surgery to not be able to happen.
Quote -
I just had a teaspoon of hummus with a teaspoon of avocado topped with a teaspoon of greek yogurt and it. was. GLORIOUS. I'm four days out and my surgeon gave me the greenlight to work in small amounts of pureed food.
-
I am 6 weeks post op as of yesterday. I had gastric sleeve. I have been unable to keep food down and have been vomiting. I am taking medication for acid reflux and something to help my stomach empty the acid.
I keep having this white foamy stuff come up. I am taking medication for nausea and drinking coconut water.
I am ready to feel normal.
-
Just deleted all of my food delivery/ordering apps and unsubscribed from several restaurant emails. I start my pre-op diet next week- unsure what that will look like until I meet with my dietician on Monday, but I want to be prepared for success. Let's go!
-
FYI. I'm going to discuss poop! I'm a Registered Nurse x16yrs. It's possible this might be to much information for some but I'm not gonna sugar coat my info/experience. I hope some find this much detail helpful.
Post op gastric sleeve 8 days out. The first day/night was AWFUL. I believe the majority of discomfort was from all the gas placed in the abdomen during surgery. Day 3 I started have less pain from the gas yet the spasm/pulling/tightness in right lower quadrant of abd. continues to this day (maybe a 4 on the pain scale w/ 10 being worst). I recommend WALK, splint your abdomen w/ a small pillow to cough/sneeze/laugh/try to have a bowel movement!
Speaking of bowel movements, my Doctor did not have me do a liquid fast 2 wks prior to surgery, only 24 hrs prior to day of. I was unable to pass gas or have a bowel movement until day 6 and that was with the help of Miralax on day 5 ( note I did take the pain med's/Lortab the first 3 days). I have no problem taking in H2O as I'm a water snob so this wasn't the issue. FYI. Narcotics can increase constipation. I recommend the Miralax, I purchased individual dose pkg's which make it simple to take on the road/convenient. Bowel movements should return to pre surgery consistency if not discuss w/ your MD.
It was difficult to urinate ( minimal volume/stream) the 1st 3 days as well, I assume due to gas and swelling in the abd. cavity, 8 days out and the all things back to normal in that department.
No appetite, only thirst first 3 days. I started the Protein shakes my local health food store offered NutraBio 100% whey protein iso. 25 grams protein in one scoop and it tastes clean no after taste/grit. I started to notice a desire to eat on day 3. I found heating up Lipton soup mix or ckn soup from a can and straining out the solid bits extremely fulfilling. Now day 8 I want to have something of substance in my belly. I'm not sure if it's hunger or habit. I am still cooking meals for my family. I bought some ice cream last night and that made a huge difference in my attitude/energy/outlook. I've noticed many different diet recommendations throughout my research in regards to the liquid phase of the diet. My surgeon wants everything low carb, low fat, calories 700-900. That is a bit extreme for me I beleive. I've already gone back to work (day 5/modified w/ no lifting over 15 pds) and couldn't make it through the day on that limited amt of calories. I've been blending canned soups to liquid consistency the last few days, loads of yogurt, popsicles and yes protein shakes. Tonight I needed something with richer consistency so I made myself a small bowl of mashed potatoes maybe 2oz. I felt so Satisfied and afterward, the idea of another week on a Liquid diet didn't seem so disappointing/unattainable.
The most dramatic changes I've noticed to my body since having the surgery is the overall inflammation/bloating in my face/abdomen is 70% resolved, my skin is 90% clearer and I don't feel the need to take my bra off the second I put it on ( strange I know). I am thrilled with my choice to have this procedure thus far. I feel much better when I listen to my body and not just blindly follow the strict eating regimen ordered by my MD. I'm not encouraging anyone to go against your MD's recommendations but for me, listening to my body and making small adjustments is making this journey more positive/manageable.
To date I've lost 13 pds and it's only day 8 post op.
-
Hi everyone, I have been reading posts here for a while and have learned so much from all of you. My VSG takes place on 31st May and after looking forward to this for so long I am now experiencing a lot of anxiety about it. I am worried that I could be one of the very few that will experience a leak and I'll end up having to stay in hospital for months or worse! I'm not worried about the pain or not being able to eat and drink my favourite foods (well, that's not entirely true, I do wonder how I'll cope in social situations as I am not telling anyone apart from my husband, who is also scheduled for VSG one month after me, and my grown-up children. What I am REALLY worried about it not working for me. I have yo-yo dieted my whole adult life and use to find it relatively easy to lose weight, Not any more! Over the past couple of years I have tried many VLC diets and lost nothing, or even put on weight! So, my concern is that having the sleeve that literally forces me to controls the amount I can eat will be no different to a VLCD. I am 56 and I know that it is harder to lose at my age. I am praying with everything I have that getting the sleeve will do something miraculous to change my sluggish metabolism that will help me lose this weight! Any insight would be much appreciated.
-

Hi I quite understand your anxiety. I had it too just three days before my Op which was on Thursday. I am now out the other side and SO glad that I did not lose my nerve. I am at home again and just taking it easy. I was so nervous but my Friends and Family have been so supportive. One tip take loose pyjamas into the Hospital with you. I am so glad I took mine. Makes you a lot more comfortable. Good luck and just start imagining the new post op you. I also if it helps had a supply of protein drinks at home ready for the first couple of weeks. I have protein lemon water and also bought some spray vitamins which have been so good as I cannot go back to my gummy vitamins for a couple of weeks. I am on day three and made myself a yogurt and semi skimmed milk smoothie with liquidised blue berries strained through a sieve. I have made enough for two portions . Dead easy and so much nicer than some of those flavoured low fat yogurts. We are all thinking of you . Honestly I have had worse operations xx
-
aussiescot reacted to this
-

Ah, you are a treasure to respond to my rambling anxieties! I'm new to this forum and only just found your reply! I'm so glad you got on ok and are out the other end! I have protein powder and protein water powder in a couple of flavours at the ready. I must try and fins spray vitamins. I've never heard of that before but it sounds like a great idea, especially when you can't eat your gummies. I have chewable multivitamins so I wonder if I'll be allowed to take them? Ou, thank you also for the advice about tge loose jammies, I will definitely take them. Take care and keep in touch. x
-
-
I am now 52 years old and I have had a Lapband in Monterrey, Mexico in 2009 and a Bariatric Sleeve in Tijuana in 2017. With the Lapband I lost maybe 2-35 pounds and gained it right back and then some. It was not an adjustable band it was just a ring around my stomach according to the surgeon (who had a hard time removing it) when I did my Gastric Sleeve. When i decided to do the Bariatric Sleeve in 2017 my weight was 348 pounds and I was struggling with walking, breathing, no energy, buying/finding clothes and I was put on 2 blood pressure pills and a cholesterol pill. My Sleeve surgery went great and I was feeling so good down to 321 and loving it (I didn't even mind the liquid diet I was still on) and then I started to feel sick 2 weeks out of my Sleeve surgery and it ended up being a stomach leak on the staple line. I struggled with drains for about 2 years and finally in December of 2019 i was drain and leak free. After all that I was down 100 pounds and was weighing 248. When I had the drain I never exercised I would just walk a bit with friends every other day maybe until we didn't because life got busy or I got sick again. At the hospital I found that I was now lactose intolerant and I have not found any protein shakes I can drink without feeling sick to my stomach. I have regained about 26 pounds and i just want input on how to lose weight since i am not on any particular diet and eat all kind of bad food until I am full ( i would love some recipes or a daily menu). I have been considering the Gastric Bypass since I have horrible reflux and have been researching the pros and cons and would appreciate any input.
-

You might try the Thrive Lifestyle Mix. Its a protein shake but it does have some carbs. I have a problem with protein shakes. They make my stomach hurt. I recently started the Thrive 3 step which is a vitamin (in capsules) and a skin patch and a shake mix. The shake works for me and I think the reason why is because it has digestive enzymes in it. This makes it a lot easier for your stomach to break it down. It has amylase, bromelain, cellulase, protease, lipase, papain, and protease. Its like taking a whole digestive enzyme capsule with your protein shake, but its all in an individual serving envelop and you mix it with whatever you want. I mix mine with either water or almond milk, but you could mix it with soy milk if you wanted to do that. It is the easiest to digest nutrition shake I've ever done. If you decide you want to try it. I know a gal who will probably send you a sample or two. I actually have enough packets of this that I could send you a couple packets to try if you message me your address.
-

-
-
Anxiety is through the roof right now and I vacillate between "I want to eat and self-medicate with food!" and "I'm too hyper and nauseous to eat right now! Btw, where is the caffeine, b*tch?!"
This seems to cancel itself out calorie-wise. Two more weeks of this crap. Then I'm going to sleep for three days straight I guess. Or maybe not.
-
I am having a very fast heart rate after my surgery post op surgery (sleeve) my rest heart rate is around 94-110 - sometimes even when i walk it goes up to 145!
it’s literally killing me - i just had the heart mointer placed but I’m not sure what to do about it . I’m post op 6 months i was 230 and now I’m 189 and at a stand still!
probably my fault i still have a healed time eating food especially protein - i do workout but i know food is important (previous body builder )



























(edited-Pixlr).jpg.0b6e5035c556e9ad95d0b0e0b7c90d6f.jpg)