
SleevedK
-
Content Count
44 -
Joined
-
Last visited
Posts posted by SleevedK
-
-
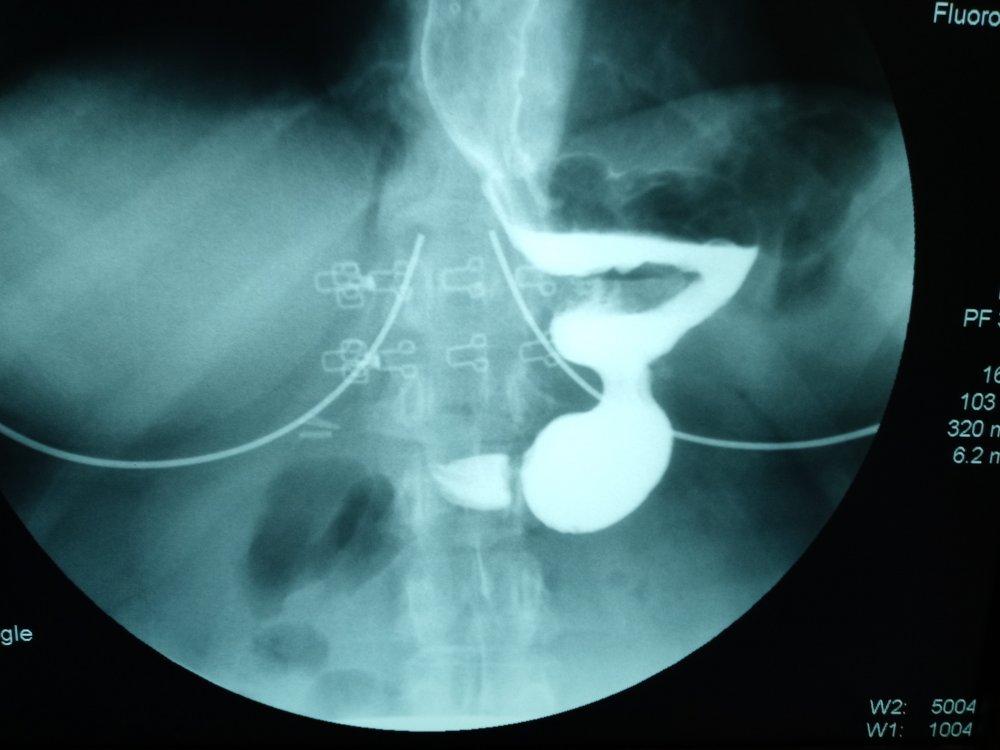
5 hours ago, escape_pinacolada said:UPDATE: I was able to see another doctor in California. Her first question was "why haven't you had a by-pass yet"? She did surgery and loosened the "fix" that Dr. Ganser did, but after 3 months I was having the same issues. Vomiting, nausea and severe pain when eating or drinking especially Water. The doctor in Sacramento did a new upper GI and said I need a by-pass, due to how my stomach is shaped after my surgeries with Dr. Ganser. She let me know that she can do the surgery to the by-pass, but she wants 6000.00 up front as well as my insurance payment and my 20%. I am not able to afford that, so I have to look for another surgeon in Reno. I also have an issue with finding a surgeon that uses the proper facilities (a Center of Excellence...). Frustrating and disheartening. It has been 6 years of pure misery. When it rains it pours. I attached a picture of what my stomach looks like, each time I eat, the food gets stuck in the hard 90 degree turn and then I am sick and vomiting, nausea and pain.
I am so sorry that you are suffering with all these awful complications and having trouble getting help, but I hope that now that you know what needs to be done to fix it at least it helps to know there is hope that things will get better. Thank you for telling everyone about this so that people realize that this surgery is not something to take lightly. Everyone talks about how the sleeve is such a safe surgery, but the truth is that it CAN have life-altering complications.
KateinMichigan and lizonaplane reacted to this -
What did you end up finding out? I hope that you are doing okay.
-
3 hours ago, Abbie_tom said:I’m now 9 months post op and down 90lbs. I was told that my GERD would subside about a month after surgery. It has not. They just did an X-ray and found a hiatal hernia and severe esophagus reflux. I’ve not spoken with my doctor yet (just read the results) but is there a fix for this? I did not have the hernia prior to surgery (was checked 4 times).
I am sorry you are dealing with this. It is an awful problem. A lot of surgeons will tell you to convert to bypass for bad reflux and a hiatal hernia, but you can try fixing the hiatal hernia and see if that works. For some people, just fixing the hiatal hernia is enough to help the reflux. Since most of our stomach is gone, we can't have a Nissen fundoplication (the usual procedure to fix a hiatal hernia and control acid) but they can still just pull the stomach down into your abdomen and stitch the diaphragm closed. The main reason that is not always their first choice is because that may have a higher failure rate. Another option if your esophagus is strong enough for it would be to get a Linx device, since that seems to help keep hiatal hernias from coming back too.
-
Yep, I have GERD and a hiatal hernia. I am still trying to weigh the options on how to deal with it. Knowing what I know now, I wish I had never had bariatric surgery at all - in MY case, I think I would have been happier and healthier without surgery, because my weight wasn't causing me any health issues yet and I just gave myself new problems with the surgery. If I was in fact dealing with health issues from the weight, now I feel like I might have been better off just doing the gastric bypass from the start.
Tracyringo and KateinMichigan reacted to this -
1. Did you feel the same way? Yes, I was not totally sure about getting the sleeve, but I ignored my doubts and went through with it anyway.
2. Are you glad you did it? No. I do regret it.
3. Do you have any regrets? Yes. I now have a hiatal hernia and GERD that affect my quality of life. The hiatal hernia came AFTER the sleeve - I didn't have one beforehand.
I didn't realize at the time that I had the sleeve that the shape of the sleeved stomach makes it prone to herniate, that if it does herniate that it can cause very significant symptoms even if it is a "small" hernia, and that permanently fixing a hiatal hernia after the gastric sleeve is not easy (hence many surgeons will tell you to just convert to a gastric bypass if you get a hernia after the sleeve). 4. What’s one thing you wish someone had told you before you had surgery? I wish that someone had simply explained to me the problems that hiatal hernias can cause, that the gastric sleeve makes it much harder to surgically fix a hiatal hernia than it is if you still have your normal stomach, and that your quality of life can be ruined if you are one of the unlucky ones who has a lot of symptoms from it.
I wish someone had told me that there was a real risk that I might end up being forced into converting to a gastric bypass because the sleeve caused problems.
I know that pre-op people don't love hearing about regrets or the problems, but the truth is that I was better off before the surgery. Sure, I was fatter, but I was pretty healthy in spite of that and my weight was not affecting my quality of life.
I desperately wish I could go back in time and tell my surgeon not to do it. The surgery works for a lot of people, but some people are worse off after it. If you aren't SURE you want the surgery, and especially if you are not willing to accept the risk that you might end up with health issues that force you to convert to a gastric bypass later, then I would advise not rushing into it. Wait until you are sure. -
Do you know if you are a candidate for Linx, JRL? That is an option for fixing the hernia and LES, *if* you have enough esophagus motility for it.
I would definitely talk to a surgeon who does Linx before I would agree to a bypass.
It is hard for me to accept the idea of being forced into a bypass when I really regret ever getting bariatric surgery to begin with. I feel like I am worse off this way than I would have been with my original stomach and the extra weight.
KateinMichigan reacted to this -
Thank you for bringing attention to this issue. People who haven't lived with significant GERD often don't understand how serious it can be and how it affects quality of life. We need to find solutions to this problem. Now that so many people have gotten the sleeve, there will be an explosion of people affected by the nasty form of GERD that can happen post-sleeve, and not all of them are good candidates for the bypass. I feel like doctors push people to convert to bypass whenever there is an issue with the sleeve because that is something they are familiar with and has fairly predictable complications. However, I have seen so many stories of people who converted to bypass but then ended up with new problems or still had reflux even then.
There has to be a better way to deal with this problem.
Can I ask, how have you managed to cope with the awful GERD all this time? What do you do in order to get through the day? Have you developed Barrett's esophagus? -
I also found some articles by Dr. Craig Chang, who seems to be very aggressive about repairing hiatal hernias in his bariatric patients and apparently has had good results. Perhaps he is worth consulting with as well?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4754198/
https://www.sages.org/meetings/annual-meeting/abstracts-archive/sleeve-gastrectomy-with-reinforced-laparoscopic-hiatal-hernia-repair-outcomes-and-clinical-experience/ -
I saw this webpage for Dr. Elias Darido, who appears to be very knowledgeable about the sleeve and says that in many cases a hernia repair alone will stop the reflux. He will do virtual consults online. However, I have not yet found anyone who has actually seen him as a patient, so I don't actually know much about him.
https://houstonsleevesurgeon.com/category/acid-reflux-and-heartburn/
I also found out that Dr. Keshishian, who I know is pretty well known in the WLS world, has experience with repairing hernias after sleeves:
https://www.dssurgery.com/laparoscopic-hiatal-hernia-repair/Bariatricwarrior reacted to this -
I am so glad that you mentioned that Dr. Jossart is experienced in dealing with this issue. I will need to look into that. Did you have to make an appointment with his office staff to talk to him?
I am sorry that you are suffering with these issues too, but I am also glad that you are here and talking about what you have learned. It is so nice to hear from someone else who is interested in this topic and taking action to try to figure it out. This is such a difficult problem because it seems like there aren't a ton of people who have dealt with it so you feel kind of alone struggling to find help with a complicated problem that even many doctors don't seem to understand very well. To be honest, I desperately wish that I had never had the sleeve, because I didn't understand at the time what trouble it could lead to, and I NEVER wanted a bypass under any circumstance. I wish I had made it more clear to my doctor at the time that I did not consider the bypass an option and maybe then she would not have done the sleeve.
Here are a couple of other leads that I have found that you might want to check into:
Dr. Kenneth J. Chang at UC Irvine is doing research into an experimental method of controlling GERD with an endoscopic procedure that can be done post-sleeve.
https://www.ucihealth.org/find-a-doctor/c/kenneth-chang
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6133678/
Dr. Olaya I Brewer Gutierrez at Johns Hopkins is apparently close to starting a clinical trial using a similar endoscopic procedure:
https://clinicaltrials.gov/ct2/show/NCT04771247 -
I would love to hear what he says to you about it, KateInMichigan! It would be great to know if this is really a viable option.
-
10 minutes ago, Yvonne Cepeda said:I had my GBP 15 yrs ago, just had a Rivision
Why did you have to have the revision? I hope it helps you feel better.
-
My situation is a little different (GERD and hiatal hernia, but sleeve seems okay) but here is what I would suggest based on what I have learned trying to understand my problems.
It might be worth getting a second opinion from a surgeon in a different practice who is willing to look at your upper GI imaging and tell you if they think the sleeve looks properly shaped or not. I have been reading this doctor's webpage where he talks about how, in some cases, a misshapen gastric sleeve can aggravate GERD: https://houstonsleevesurgeon.com/category/acid-reflux-and-heartburn/
If you are having significant GERD, you should probably get on meds for that and see if that is enough to control it. When I was reading about this, I did see one study that talked about how, for some post-sleeve patients, the GERD gets better after about 3 years or so because your stomach becomes more "compliant' by that point (and then there is not as much pressure in the sleeve to push the acid up), so if the GERD is controllable with meds, you could try waiting it out and see if it gets better. If it doesn't get better, or if it is not responding to the meds. then you have to decide if you want to get an RNY, or if you want to try the Linx, or possibly ask your doctor about this new procedure I recently learned that some doctors are trying for those of us with sleeves who are having GERD: https://www.sciencedirect.com/science/article/abs/pii/S000296102030814XCia2020 reacted to this -
So sorry that you are dealing with these problems. I have dealt with GERD of various intensities since I had the lap-band many years ago (and since I switched to the sleeve) so I can sympathize with how terrible it can be.
I hope that the nodule results come back benign.
Here's what I have been able to learn about the situation of post-sleeve GERD:
Switching to an RNY is the best-studied option and therefore that is what many people will tell you to do, because we know it works to get rid of acid for MOST people (some people will still have problems even then, but most do not).
The Linx procedure is a newer one and there isn't yet a lot of great data on how post-sleeve people do with it. However, it is supposed to be reversible, so I think the main risks you run with getting the Linx is that #1: if it doesn't work well, you then have to go through another surgery to remove it and get the RNY and #2: there is a chance of having to deal with an erosion or scar tissue that might make the removal more complicated. If you do get the Linx, I'd definitely try to find someone who has done a lot of them and is confident about doing it. Since it is a new option not every surgeon will have done a lot of them.
Another option you may want to ask your doctor about is this procedure called a "ligamentum teres cardiopexy". Basically, they just take a ligament hanging off your liver and loop it around your esophageal sphincter to strengthen it in order to try to stop the GERD. This is something new that some surgeons are doing for sleeve patients who have GERD (since we can't have a fundoplication like "normal" people and many of us don't want the RNY). To me it seems like a less complex and easier surgery than the other options, so I am going to ask my doctor about it. Here are some articles about it if you want to show them to your surgeon:
https://www.sciencedirect.com/science/article/abs/pii/S000296102030814X
https://pubmed.ncbi.nlm.nih.gov/31175555/
Good luck with finding an answer. -
I think we definitely need to be honest that these surgeries can cause problems and I encourage long time surgery vets to be open about what they have dealt with.
I started out getting the lap-band in 2003. I read a ton of patient experiences on email lists, ObesityHelp, and online forums. I read medical journal articles about it. I read about how it had been used in Australia with good results for some time before that. I thought I knew what I was getting into. Most people at the time really thought that the band was a low-risk, easily reversed surgery.
By the time I had my band removed over 10 years later, it was clear that it is NOT a good surgery for most people and that the majority of people end up having problems from it. What seemed like the safest option at the time ended up being probably the worst option for most of us. Now most surgeons no longer put bands in at all.
When I had the band removed, I switched over to the gastric sleeve, because again it seemed like the lowest risk option. Now I am dealing with a hiatal hernia and learning that it is pretty common to tell sleevers who have GERD or hiatal hernias after surgery that they should just get an RNY. I never wanted an RNY because I was scared of the potential complications. I am still hoping and praying there will be another option, but it is scary to think that I might be forced into yet another surgery with yet more possible complications. While I know many people do great with the RNY for many years, I also know people who ended up with awful complications and have suffered. I am tired of taking these risks.
Having 5 year data on patient outcomes is great for a research study, but for the patient that is not necessarily enough. When it is a permanent surgery that you have to live with for the rest of your life, it is not much consolation to know most people do great at 5 years if you are one of the unlucky ones who has problems 10 or 15 years later. -
I just recently found out that there is a surgical procedure that might be helpful for those of us who have a hiatal hernia and GERD after the sleeve to repair the problem without having to convert to an RNY. It is called "Cardiopexy with Ligamentum Teres" (basically they wrap part of a ligament from your liver around the esophagus to reinforce the lower esophageal sphincter)
Here is a recent article that discusses this technique if any of you want to show it to your doctor and get their thoughts.
https://www.americanjournalofsurgery.com/article/S0002-9610(20)30814-X/fulltext#gr2
And here is a video of a surgery performing it:
https://www.youtube.com/watch?v=t_SbDqhueRU
Have any of you had this done, or at least been able to talk to your surgeon about it? It seems like this is not yet being done widely, so I would welcome any info any of you have about it. If you have had this done or know someone who did, what were their results like? Thanks! -
I’m sorry you are going through this. I don’t have personal experience with this procedure but I have had complications with the procedures I did have and I know it is hard.
You may want to see a bariatric surgeon to see if they can do some kind of revision procedure on you. what you describe sounds similar to a procedure that used to be done that’s called “vertical banded gastroplasty” and I know that many people who had problems with that surgery ended up having revisions.
It sounds like this issue should be fixable. Hope you find answers soon. -
Have any of you dealt with a hiatal hernia AFTER getting sleeved? What ended up happening?
I am currently dealing with this. I haven’t yet found out what my surgeon wants to do, but I am afraid that I will be told the only option is to convert to RNY, and I absolutely do not want that. Have any of you had luck with simply repairing the hernia and keeping the sleeve instead of converting to RNY?
Do any of you have suggestions on doctors who may be experienced at dealing with this problem?
i appreciate any advice since it is hard to find info on this problem. It seems like tons of people have hernia repairs at the time they have the sleeve done but it seems less common to have it come up later.





Sleeve to bypass revision with arthritis
in Revision Weight Loss Surgery Forums (NEW!)
Posted
I am sorry you are dealing with this. If they won't do a bypass, the other options would be to just repair the hiatal hernia and see if that alone will stop the reflux, or to get a Linx device put on your sleeve: https://www.jnjmedicaldevices.com/en-US/campaign/LINX-GERD-relief
If you feel like you're not totally convinced you want to get the bypass then I would talk to the surgeon about those other options. Just doing nothing isn't an option, since bad reflux is such a miserable problem to deal with and can be so dangerous.